HRT, breast cancer, and the framing of risks
As of the 23rd May 2022 this website is archived and will receive no further updates.
understandinguncertainty.org was produced by the Winton programme for the public understanding of risk based in the Statistical Laboratory in the University of Cambridge. The aim was to help improve the way that uncertainty and risk are discussed in society, and show how probability and statistics can be both useful and entertaining.
Many of the animations were produced using Flash and will no longer work.
The way that risks are 'framed' can make a big impression on their apparent magnitude. The controversy following the recent report by NICE on hormone replacement therapy (HRT) provides a fine example.
HRT is known to increase the risk of some cancers, and the Daily Mail reported claims that these risks were not given sufficient attention by NICE. In particular, the journalist quotes Professor Val Beral as saying
‘About one million UK women are currently using hormones for the menopause, and among them about 10,000 extra breast cancers are estimated to occur in the next ten years … [and] about 1,000 extra ovarian cancers.’
The Daily Mail article immediately goes on to say
But the NICE guidance says that out of 1,000 women taking HRT for five years, there would only be six extra cases of breast cancer and 1.5 additional cases of ovarian cancer.
The journalist is clearly suggesting the NICE are understating the cancer risks from HRT.
But let's look at these two risk statements more carefully. The first says that 1 million women taking HRT will lead to an extra 10,000 breast and 1,000 ovarian cancers over 10 years. If we scale this down to 1,000 women taking HRT, it is equivalent to 10 extra breast and 1 extra ovarian cancers over 10 years, or 5 extra breast and 0.5 extra ovarian cancers over 5 years.
But in the second statement, NICE are reported as saying that 1,000 women taking HRT for 5 years will lead to 6 extra breast and 1.5 extra ovarian cancers, which are higher than the risks claimed by Professor Beral.
So why does the first description of the risk give such a strong impression of being worse than the second?
This is all down to the 'framing'. By using a large denominator (a million women), the number of cancers is larger and the risks look bigger – this is the classic idea of ‘ratio bias’. Whereas the second description says an extra 5 breast cancer cases out of 1,000 women - equivalent to one extra case for every 200 women taking HRT for 5 years - which does not feel so large.
So, rather mischievously, what could we do if wanted the breast cancer risk to look even smaller? We might consider the baseline lifetime risk of getting breast cancer, which Cancer Research UK say is around 13%. Taking out the 20% of breast cancers occurring in women under 50, we might predict that 10% of women, at the age they might take HRT, will later get breast cancer.
So, very roughly, out of 200 women who might take HRT, we would expect around 20 to later develop breast cancer. On the other hand, if 200 similar women took HRT for 5 years, we would, from the numbers given above, expect one extra case, or 21 cases in all. This comparison can be shown using the icon arrays below.
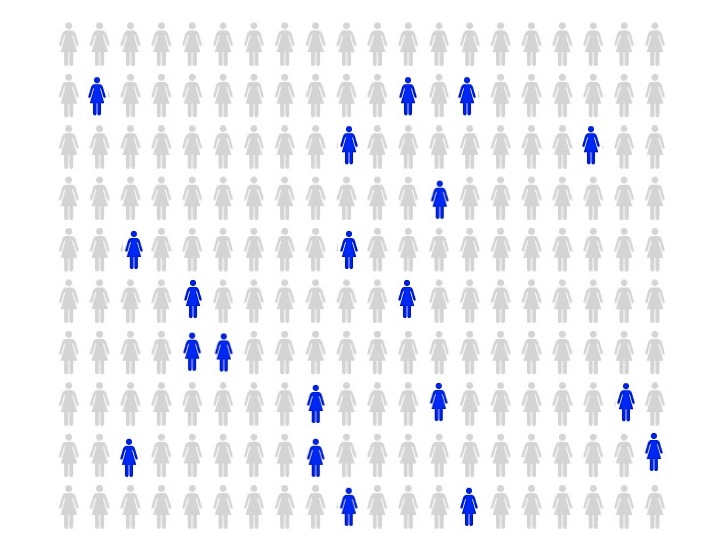
Out of 200 women in their 50s, we would expect 20 to eventually get breast cancer [blue]
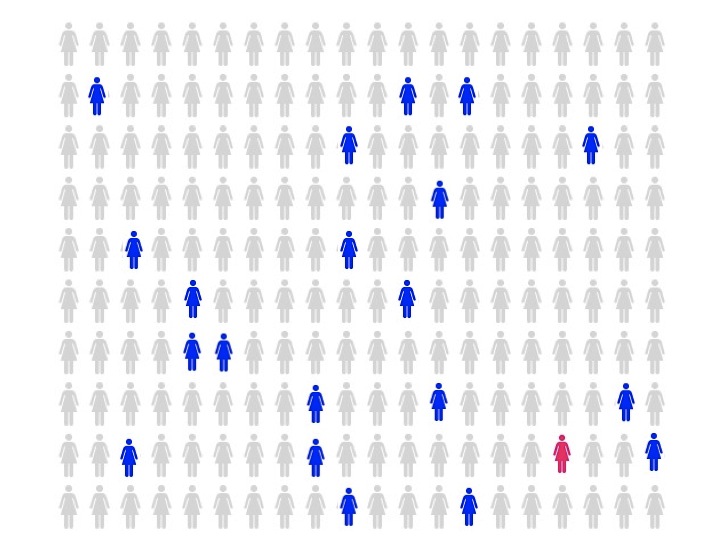
Out of 200 women in their 50s who take HRT for 5 years, we would expect 21 to eventually get breast cancer [blue and red]
The extra red icon represents the increased risk from taking HRT for 5 years - this may, or may not, seem a reasonable chance to take for women who have severe symptoms that can be relieved by HRT.
So much for ‘facts’ – now for some personal, subjective opinion about these issues.
- Describing risks in terms of its effects on populations, for example the million women taking HRT, is sensible for public health discussion but is utterly irrelevant to the individual decision a woman has to make. If discussing a treatment choice with an individual woman, it appears to me be a manipulative framing of the risks.
- Picking on a single adverse event, even one as important as cancer, is no basis for risk communication and again seems a manipulative form of communication.
- In a complex decision such as whether to take HRT, in which a woman’s feeling about her symptoms are so important, she should be presented with the potential harms and benefits communicated in a balanced and uniform way. The form of communication should be appropriate to her level of numeracy and wish to engage with the evidence.
- She can then make up her own mind, based on principles of shared care and informed choice. Of course, if she wants to defer to doctorial advice, that is completely fine.
End of diatribe.
- david's blog
- Log in to post comments

Comments
AmandaKelly
Fri, 02/12/2016 - 10:29am
Permalink
HRT can also boost the risk